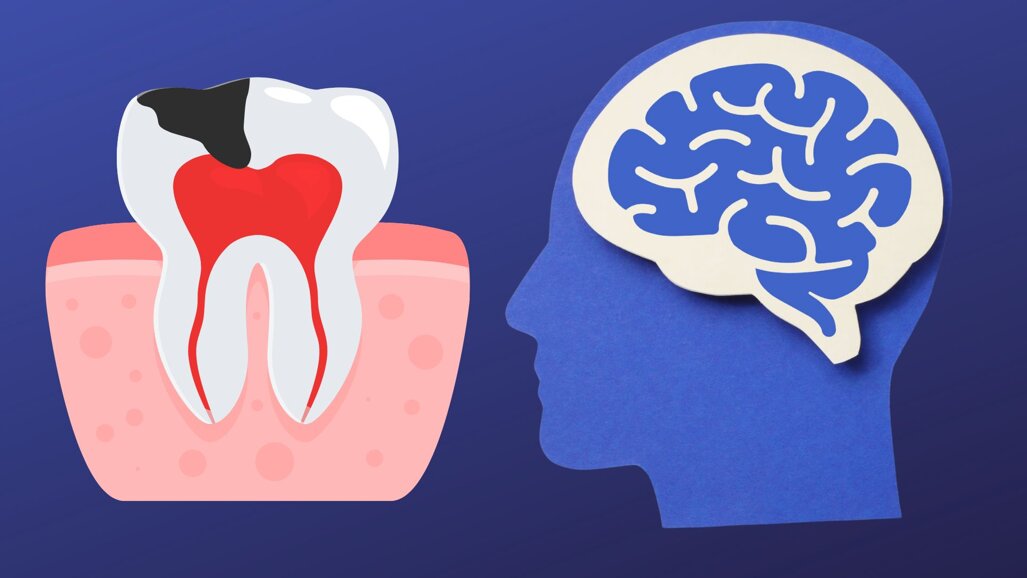
A groundbreaking study conducted by researchers at Atatürk University in Turkey has shed light on the far-reaching impacts of early childhood caries (ECC) on children’s mental and social-emotional development. Published in December 2025, the recent study emphasises the importance of timely and effective management of ECC to protect not only physical health but also children’s cognitive and emotional well-being.
ECC: A Growing Public Health Concern
ECC, defined by the American Academy of Paediatric Dentistry (AAPD) as the presence of decayed, missing, or filled tooth surfaces in children under 71 months of age, is a widespread issue affecting children globally.
A review from August 2025 in The International Dental Journal reports an alarmingly high prevalence of ECC in the Asia-Pacific region. Seven out of ten children under the age of five are affected, indicating a significant dental health concern for young children in these areas.
Beyond pain, infection, and functional impairments, ECC also leads to developmental delays and social exclusion. This study directly examined the association between ECC and mental development, providing deeper evidence in this research area.
The Study
The research involved 150 children aged 36–48 months, categorised into three groups: those with severe ECC (sECC), those with ECC, and caries-free children. The study included 48% girls and 52% boys.
All children were evaluated using the Turkish versions of the Ages & Stages Questionnaire (ASQ®-TR) for mental development and the Ages & Stages Questionnaire-Social Emotional (ASQ®-SE-TR) for emotional well-being.
The ASQ®-TR measured communication, gross motor skills, fine motor skills, problem-solving, and personal-social development. The ASQ®-SE-TR measured social-emotional skills, self-regulation, compliance, affect, and peer interaction.
Key Findings
- Children with sECC in all age groups had a higher risk of developmental delays and social-emotional problems than caries-free peers.
- Notably, 48-month-old children with sECC faced the highest risks for developmental delays and caries. Two out of five had this risk. One out of three had lower developmental skills.
- At 42 months, children faced the highest risk for developmental disability.
- Boys had higher risks of developmental delays and problems than girls in all age groups.
- The girls showed a higher risk for socio-emotional developmental delays, except in the 36-month-old group, where scores were low.
- The research also emphasised the effect of parental education and socioeconomic status on development. Children with less-educated parents were more likely to have developmental delays and social-emotional challenges.
Clinical Implications: What Can You Do as a Clinician?
The study emphasises the importance of early intervention and preventive strategies to address ECC. One of the most effective ways to evaluate young children at risk of ECC is to use a multidisciplinary approach.
Key paediatric care requires early intervention, preventing oral disease, managing eruption and space issues, correcting adverse oral and breathing habits, addressing early orthodontic needs in cases of craniofacial anomalies, supporting nutrition and respiratory health, and monitoring posture. Also, prioritising the child's mental and cognitive development.
Applying this in practice enables clinicians to deliver scientific and practical support for children's growth and development. Researchers call for comprehensive oral health programs to protect children during critical developmental years and enhance their quality of life.
What’s Ahead?
As the first study of its kind to use standardised screening tools such as ASQ®-TR and ASQ®-SE-TR, it opens the door to further research in this critical area of pediatric health.
This study marks an important step in linking oral health to children's mental development. A multidisciplinary approach is needed to tackle ECC and support mental and social-emotional development. Addressing ECC early enables dental professionals to secure healthy smiles and brighter futures worldwide.
References:
- Dereli̇oğlu, S.Ş., Özkan, Ç., Gökdaş, B.P. et al. Impacts of early childhood caries on the mental development. BMC Oral Health 25, 2005 (2025). https://doi.org/10.1186/s12903-025-07328-w
- Faith Miaomiao Zheng, Chun-Pin Lin, Olabode Ijarogbe, Elham Kateeb, Hiroshi Ogawa, Syed Mahmood Shah, Fernando Fernanodez, Ting-Chen Chen, Ting-Yi Renn, Chun Hung Chu, Wei-Jen Chang, Managing Early Childhood Caries in Asia-Pacific Region, International Dental Journal, Volume 75, Supplement 2, 2025, 100945, ISSN 0020-6539, https://doi.org/10.1016/j.identj.2025.100945
- Qi Su, Zhiying Zhou. Multidisciplinary management points in early childhood treatment.Journal of Clinical Pediatric Dentistry,2025,49(6):22-31 DOI:10.22514/jocpd.2025.123
Topics:
Tags:
GHAZIABAD, India: Nearly half of all children in India have early childhood caries (ECC), and research shows that reducing ECC incidence requires the ...
PHILADELPHIA, US: It was previously believed that Streptococcus mutans was the main microorganism responsible for dental caries. However, in a recent study,...
The last decade has witnessed a global rise in antibiotic resistance, creating substantial challenges for healthcare systems worldwide. While the primary ...
This guest editorial comes from Dr. Wenyuan Shi, Chief Scientific Officer and Chief Executive Officer of The Forsyth Institute – the only independent ...
Early Childhood Caries (ECC) is a significant concern. Geo-maps have been extensively used abroad for presenting epidemiological data based on caries risk. ...
Two young pediatric dentists describe the emerging philosophies and concepts in Pediatric dentistry. What pediatric dentistry looks like, now & beyond 2020....
HELSINKI, Finland: Studies that link oral infections with systemic diseases and conditions have been going on for a long time. A recent Finnish study, after...
BENGALURU – "PEDO CARIE Exploring ECC" is the theme of the 14th Indian Society of Pedodontics and Preventive Dentistry National Postgraduate...
The Oral hygiene day celebrated every year on the 1st of August, was introduced to commemorate the birth anniversary of the doyen of Indian Periodontics and...
Live webinar
Tue. 24 February 2026
11:30 pm IST (New Delhi)
Prof. Dr. Markus B. Hürzeler
Live webinar
Wed. 25 February 2026
1:30 am IST (New Delhi)
Prof. Dr. Marcel A. Wainwright DDS, PhD
Live webinar
Wed. 25 February 2026
9:30 pm IST (New Delhi)
Prof. Dr. Daniel Edelhoff
Live webinar
Wed. 25 February 2026
11:30 pm IST (New Delhi)
Live webinar
Thu. 26 February 2026
6:30 am IST (New Delhi)
Live webinar
Tue. 3 March 2026
9:30 pm IST (New Delhi)
Dr. Omar Lugo Cirujano Maxilofacial
Live webinar
Wed. 4 March 2026
6:30 am IST (New Delhi)
Dr. Vasiliki Maseli DDS, MS, EdM



 Austria / Österreich
Austria / Österreich
 Bosnia and Herzegovina / Босна и Херцеговина
Bosnia and Herzegovina / Босна и Херцеговина
 Bulgaria / България
Bulgaria / България
 Croatia / Hrvatska
Croatia / Hrvatska
 Czech Republic & Slovakia / Česká republika & Slovensko
Czech Republic & Slovakia / Česká republika & Slovensko
 France / France
France / France
 Germany / Deutschland
Germany / Deutschland
 Greece / ΕΛΛΑΔΑ
Greece / ΕΛΛΑΔΑ
 Hungary / Hungary
Hungary / Hungary
 Italy / Italia
Italy / Italia
 Netherlands / Nederland
Netherlands / Nederland
 Nordic / Nordic
Nordic / Nordic
 Poland / Polska
Poland / Polska
 Portugal / Portugal
Portugal / Portugal
 Romania & Moldova / România & Moldova
Romania & Moldova / România & Moldova
 Slovenia / Slovenija
Slovenia / Slovenija
 Serbia & Montenegro / Србија и Црна Гора
Serbia & Montenegro / Србија и Црна Гора
 Spain / España
Spain / España
 Switzerland / Schweiz
Switzerland / Schweiz
 Turkey / Türkiye
Turkey / Türkiye
 UK & Ireland / UK & Ireland
UK & Ireland / UK & Ireland
 International / International
International / International
 Brazil / Brasil
Brazil / Brasil
 Canada / Canada
Canada / Canada
 Latin America / Latinoamérica
Latin America / Latinoamérica
 USA / USA
USA / USA
 China / 中国
China / 中国
 Pakistan / Pākistān
Pakistan / Pākistān
 Vietnam / Việt Nam
Vietnam / Việt Nam
 ASEAN / ASEAN
ASEAN / ASEAN
 Israel / מְדִינַת יִשְׂרָאֵל
Israel / מְדִינַת יִשְׂרָאֵל
 Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
 Middle East / Middle East
Middle East / Middle East
































































To post a reply please login or register