In this candid interview, Prof. Paul Abbott, a specialist Endodontist, currently the Winthrop Professor of Clinical Dentistry at The University of Western Australia, shares his wisdom gathered from his decades of experience in dental traumatology and endodontics.
Prof. Abbott, with your extensive experience in both private practice and academia, what inspired you to pursue a career in dentistry, particularly in the specialised field of Endodontics?
My interest in dentistry was sparked in high school. For many years, I had aspired to be a medical doctor, but then I discovered dentistry—partly through discussions with my own dentist at the time and partly through conversations with dental students I knew. I liked the idea of performing practical, hands-on clinical procedures, and dentistry certainly offered that, whereas medicine seemed more focused on consulting and prescribing unless one became a surgeon. In those days, dentistry was a relatively small profession in terms of the number of dentists, yet it enjoyed a high profile of honesty and professionalism within the community. Hence, I changed my mind and applied for dental school—and the rest is history! During dental school, I particularly enjoyed the theory of Endodontics and the clinical challenges it presented. There were very few Endodontists in Australia at that time, so after four years of general practice, I was fortunate to be accepted into the Endodontic training programme at the University of Adelaide under the guidance of Prof. Geoffrey Heithersay. This was a turning point in my life. Prof. Heithersay was an incredible role model, mentor, and inspiration. I was also privileged to have Prof. Rory Hume as my research supervisor. Together, they inspired the research aspects of my subsequent career.
Your tenure as Editor-in-Chief of Dental Traumatology spanned nearly a decade. Could you share some insights into the evolving landscape of dental traumatology during this period and any significant advancements that have shaped the field?
Dental traumatology is a unique area within dentistry, as it involves all the specialist fields. As Editor-in-Chief, I was exposed to research across all these specialties and had opportunities to work with experts in each field. Dental trauma remains an area many dentists find challenging, a fact highlighted by research in the past decade. These studies underscore the considerable need for ongoing education of dentists and the general public about how to respond to traumatic dental injuries (TDIs). Research also continues in areas such as tooth resorption, splinting, and emergency management of TDIs. Conservation of dental pulp, while not a new focus, has gained renewed interest, with more practitioners attempting partial pulpotomies when feasible to preserve pulp health.
With over 232 articles in refereed journals, 25 textbook chapters, and 47 newsletter articles, your contributions to dental literature are vast. How do you balance your academic pursuits with clinical practice, and what advice would you offer to aspiring researchers in the field?
I believe it’s essential to maintain a balance between clinical practice, research, teaching, and service to the profession to be an effective academic. Clinical practice is crucial for honing skills and ensuring that research and teaching remain relevant to real-world dentistry. In the earlier part of my career, I primarily practised privately with part-time university work, then later transitioned to a full-time academic role. In Australia, full-time academic dentists can undertake the equivalent of one day per week of clinical practice. Additionally, surrounding oneself with students and colleagues and collaborating with experts globally helps sustain innovation, relevance, and quality in academic pursuits. This approach ultimately aims to improve patient care and outcomes.
Your research interests encompass a range of areas within dentistry, including tooth resorption, pain control, and root canal disinfection. Could you highlight some recent developments in these areas that hold promise for improving patient outcomes?
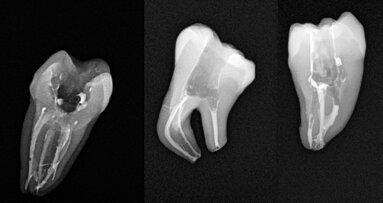
Many of these areas have seen gradual, steady progress rather than “breakthroughs,” as is typical of dental research. In tooth resorption, there remains uncertainty around managing different resorption types. We have shown that corticosteroid/antibiotic intracanal medicaments can effectively prevent or arrest external inflammatory resorption if initiated early after injuries that damage the periodontal ligament (PDL). Unfortunately, preventing external replacement resorption remains a challenge. Pain management has advanced through studies exploring pre-operative anti-inflammatory agents, local anaesthetic solutions, and injection techniques, resulting in more effective strategies for intra-operative pain. Disinfection of the root canal system continues to rely on sodium hypochlorite and EDTA, followed by medicaments like calcium hydroxide.
As former Dean and Head of the School of Dentistry at the University of Western Australia, and Director of the Oral Health Centre of Western Australia, what strategies did you implement to foster excellence in education and research within the dental community?
I was fortunate to become Dean just as we had moved into the new Oral Health Centre of Western Australia—a state-of-the-art facility with modern equipment and a new model of care, supported by government funding to subsidise treatment for low-income patients. We had the opportunity to establish policies, protocols, and workflows and to develop a new undergraduate curriculum tailored to the new facility, refining it over my seven years as Dean. We also expanded our postgraduate programmes, which boosted our research output and attracted more Masters and PhD students. I am proud of what we achieved, thanks to the dedication of our staff and students.
Having delivered over 1,000 lectures and courses in 50 countries, what do you find most rewarding about sharing your knowledge on a global scale, and how do you adapt your teaching approach to diverse audiences?
I love teaching and meeting people, especially students and colleagues. Engaging with individuals after lectures is rewarding, as I can gather feedback and answer questions. I learn a great deal through these discussions, particularly about the local context of dental practices. Understanding an audience’s background and experience level is essential, as it varies widely. Although I cover similar material for all levels, I tailor the presentation depth and adjust for local treatment approaches, materials, and instruments.
Given the rapid advancements in dental technology and techniques, how do you stay abreast of the latest developments, and how do you incorporate innovation into your clinical practice and research?
While dentistry has seen numerous advancements in recent decades, it’s crucial to remember that the fundamentals remain the same. The aim of root canal treatment is still to disinfect the root canal system. Outcomes of endodontic treatment haven’t significantly changed since the 1970s and 1980s, indicating the efficacy of past methods. Newer techniques tend to make treatment easier and quicker rather than improving results. To stay current, I attend conferences, read journals, and discuss developments with colleagues and manufacturers. I approach new tools cautiously and critically, using only those that offer genuine benefits to patients and are safe and evidence-based.
In your experience, what are some of the most challenging aspects of diagnosing and managing pulp and peri-radicular conditions, and how do you approach these challenges to ensure optimal patient care?
Pain diagnosis can be challenging, although pulpitis and apical periodontitis are relatively straightforward if all necessary information is gathered. Unfortunately, many dentists don’t use pulp sensibility tests or take adequate radiographs. Persistent apical periodontitis after root canal treatment presents another challenge, as deciding whether to re-treat can be complex. Endodontic retreatment is a major focus of my clinical work and research, and although it generally yields good results, success depends on understanding why the initial treatment failed and addressing those issues effectively.
As an Officer of the Order of Australia, you’ve been recognised for your distinguished service to clinical dentistry, higher education, and professional organisations. What motivates you to continue advancing dentistry after such a prestigious honour?
Receiving the Officer of the Order of Australia award was a career highlight and an unexpected honour, especially as it came from the community. It motivated me to continue contributing to the profession. The award was also recognition of those who supported me, especially my family, students, and colleagues. They inspired me before and after the award, and it’s been fulfilling to give back.
Based on current evidence and advancements in endodontic practice, are there any traditional methods of root canal treatment that you believe should be discontinued?
No, I believe that traditional methods should not be discontinued. Modern techniques have not shown significantly improved outcomes; traditional methods still yield excellent results. Furthermore, it’s essential for students to learn traditional techniques, as they build hand skills, and are essential for cases where modern instruments aren’t applicable.
Looking ahead, what do you envision as the future of endodontics, and what areas will likely be the focus of research and clinical innovation?
While it’s difficult to predict, I foresee ongoing development of instruments driven by manufacturers. I hope that research on disinfection agents, dental trauma, and tooth resorption continues. The terms “pulp regeneration” and “revascularisation” remain misleading, as true pulp regeneration has not been shown to occur in human or animal teeth despite decades of research. Current regenerative techniques are better termed “repair,” and much more research is needed to ensure predictable outcomes.
What are your top three book recommendations in endodontics?
My top recommendation is Andreasen, Andreasen, and Andersson’s Traumatic Injuries of the Teeth—the “trauma bible” every dentist should have. For Endodontics, I recommend Ingle’s Endodontics and Pathways of the Pulp, along with Endodontic Advances and Evidence-Based Clinical Guidelines by Ahmed and Dummer.
Lastly, if you could sum up your philosophy on life, what would it be?
I believe in doing what you enjoy and enjoying what you do. Family comes first, then friends, then work. I also think what you get out of life depends on what you put in. Whether through charitable work, pro bono treatment, or community support, we can always find ways to give back. We are privileged in our profession, and we have the ability to make a positive difference. Once you find a way you enjoy, go for it!
Editorial note:
About
Before taking a full-time university position in 2002, Dr. Abbott spent 17 years in private specialist practice in Perth and Melbourne. He was Dean and Head of the UWA School of Dentistry and Director of the Oral Health Centre of WA from 2003-2009. Prof. Abbott has lectured extensively (over 1,000 lectures and courses) in 48 countries and has published over 225 articles in refereed journals and 25 textbook chapters. He was the Editor-in-Chief of the international refereed journal Dental Traumatology from August 2015 until December 2022. He has served on editorial boards and scientific review panels of 17 other international journals.
Topics:
Tags:
Dr Giampiero Rossi-Fedele is currently a professor in endodontics at the University of Adelaide, South Australia, and since 2014 the course convener for the...
The Conceptual Hybrid Flare (CHF) technique is a novel technique developed to revolutionize the cleaning and shaping of root canals making the endodontic ...
Dr Rajiv Patel from the US will be a speaker at the upcoming ROOTS SUMMIT, which will take place from 9 to 12 May in Athens in Greece. His lecture will ...
To make the wait for ROOTS SUMMIT 2024 a little sweeter, the organisers would like to spotlight some of the speakers for next year’s edition, which will ...
As cancer treatments evolve, clinicians of all disciplines must also adapt their approaches to medical and dental treatments in order to best compensate for...
Registration for ROOTS SUMMIT 2024 is open, and the organisers would like to introduce some of the great speakers and their lecture topics for next year’s...
I start my editorial journey today as the editor of Endodontics & Biomimetic Dentistry with two topics in mind:
The exploration of biomimetic ...
Lasers were introduced to dentistry in 1965 by Leon Goldman. The first application was a failure because of excessive thermal damage. We can only wonder ...
Live webinar
Tue. 3 March 2026
9:30 pm IST (New Delhi)
Dr. Omar Lugo Cirujano Maxilofacial
Live webinar
Wed. 4 March 2026
6:30 am IST (New Delhi)
Dr. Vasiliki Maseli DDS, MS, EdM
Live webinar
Wed. 4 March 2026
10:30 pm IST (New Delhi)
Munther Sulieman LDS RCS (Eng) BDS (Lond) MSc PhD
Live webinar
Wed. 4 March 2026
11:30 pm IST (New Delhi)
Live webinar
Fri. 6 March 2026
1:30 pm IST (New Delhi)
Live webinar
Tue. 10 March 2026
1:30 pm IST (New Delhi)
Assoc. Prof. Aaron Davis, Prof. Sarah Baker
Live webinar
Wed. 11 March 2026
5:30 am IST (New Delhi)
Dr. Vasiliki Maseli DDS, MS, EdM



 Austria / Österreich
Austria / Österreich
 Bosnia and Herzegovina / Босна и Херцеговина
Bosnia and Herzegovina / Босна и Херцеговина
 Bulgaria / България
Bulgaria / България
 Croatia / Hrvatska
Croatia / Hrvatska
 Czech Republic & Slovakia / Česká republika & Slovensko
Czech Republic & Slovakia / Česká republika & Slovensko
 France / France
France / France
 Germany / Deutschland
Germany / Deutschland
 Greece / ΕΛΛΑΔΑ
Greece / ΕΛΛΑΔΑ
 Hungary / Hungary
Hungary / Hungary
 Italy / Italia
Italy / Italia
 Netherlands / Nederland
Netherlands / Nederland
 Nordic / Nordic
Nordic / Nordic
 Poland / Polska
Poland / Polska
 Portugal / Portugal
Portugal / Portugal
 Romania & Moldova / România & Moldova
Romania & Moldova / România & Moldova
 Slovenia / Slovenija
Slovenia / Slovenija
 Serbia & Montenegro / Србија и Црна Гора
Serbia & Montenegro / Србија и Црна Гора
 Spain / España
Spain / España
 Switzerland / Schweiz
Switzerland / Schweiz
 Turkey / Türkiye
Turkey / Türkiye
 UK & Ireland / UK & Ireland
UK & Ireland / UK & Ireland
 International / International
International / International
 Brazil / Brasil
Brazil / Brasil
 Canada / Canada
Canada / Canada
 Latin America / Latinoamérica
Latin America / Latinoamérica
 USA / USA
USA / USA
 China / 中国
China / 中国
 Pakistan / Pākistān
Pakistan / Pākistān
 Vietnam / Việt Nam
Vietnam / Việt Nam
 ASEAN / ASEAN
ASEAN / ASEAN
 Israel / מְדִינַת יִשְׂרָאֵל
Israel / מְדִינַת יִשְׂרָאֵל
 Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
 Middle East / Middle East
Middle East / Middle East



















































To post a reply please login or register