Periodontal health extends far beyond the confines of the mouth, reaching into the intricate ecosystem of the gut. Recent research suggests a fascinating interplay between periodontal healing and gut health, shedding light on potential avenues for improving overall well-being through periodontal treatments and healing.
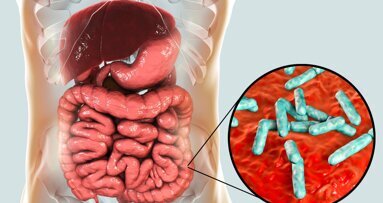
Periodontal disease is a prolonged inflammatory ailment that impacts the periodontium, which consists of the gingiva, ligaments, and bones that structurally support the teeth. The pathogenesis of periodontitis is substantially influenced by dysbiosis, an imbalance of the oral microbiome. The community of bacteria, viruses, fungi, and protozoa that are present in the oral mucosa is known as the oral microbiota. Pathogenic bacteria are the most dominant microbiota. In periodontal disease, the ratio of pathogenic to commensal bacteria is altered. An association exists between periodontitis and gut microbiome.1
Periodontal disease is related to numerous systemic health complications such as cardiovascular disease, diabetes, as well as negative pregnancy outcomes. More recently, attention has turned to the potential correlation between gut health and periodontal. The alterations in the gut microbiota can perform a key function in the growth of dysbiosis and subsequently periodontal disease.1 There is a bidirectional hypothesis that periodontitis can also influence gut health via salivary microbiota.2
Gut microflora and periodontal disease
Several latest investigations have determined that the gut microbiota holds a potential involvement in the pathogenesis of periodontitis and oral microbiome dysbiosis.1 Recent research has suggested that variations in the constitution of the gut microbiota can influence the immune system as well as inflammation, consequently affecting the oral microbiota and contributing to the onset of periodontitis. Furthermore, because saliva is consumed, which may aid in the transfer of oral microbes to the gut, recent investigations have indicated a feasible relationship between the microbiota of the gastrointestinal tract and the mouth cavity. It is conceivable that gut microbiota will reciprocally enter the mouth cavity.1
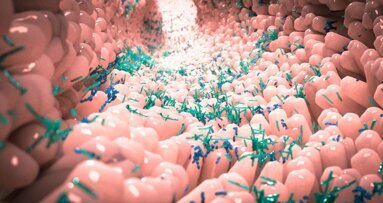
According to several studies, certain gut bacteria may protect against periodontitis, while other microbiota may make the condition more likely to occur. According to the study, there was a noteworthy distinction in the quantity of some gut bacteria, specifically Lachnospiroceae and Ruminococeae, between those who had periodontitis and those who were deemed healthy. Therefore, maintaining a balanced microbiome in the mouth and gastrointestinal system may be important for both preventing and treating periodontal disease. Probiotics and prebiotics, along with a healthy diet and consistent brushing and flossing, can assist in achieving a balanced oral and gut microbiota.1
Several recent studies have investigated this connection, aiming to elucidate the mechanisms through which PD may influence the gut microbiota and overall gastrointestinal function. The gut microbiota, a varied group of microorganisms living in the gastrointestinal tract, is essential for digestion, immune system control, and metabolic functions. Dysbiosis, which refers to the gut microbiota imbalance, is associated with health ailments like inflammatory bowel disease, irritable bowel syndrome, as well as metabolic disorders.3
In the latest research, Stool samples have been gathered from patients presenting healthy periodontium., gingivitis, and chronic periodontitis. The composition of intestinal microbiota was assessed by Illumina MiSeq sequencing. A less diverse gut microbiome was observed in patients with periodontal diseases. Many oral bacteria correlated with periodontal damage as well as inflammation had been discovered in the gut microbiota of individuals, irrespective of their periodontal status.4
Another study in 2020, investigated the impacts of periodontal therapy on gut microbiota composition in patients with chronic periodontitis. Following periodontal treatment, which involved scaling and root planing to remove dental plaque and calculus, the researchers observed significant changes in the treated individual’s gut microbiota. Specifically, they noted an increase in microbial diversity and a shift towards a more favorable microbial profile resembling that of healthy individuals. These findings suggest that improving periodontal health may have beneficial effects on gut microbiota composition.5
Beyond microbial changes, periodontal healing may also influence systemic inflammation, which can impact gut health. Periodontal disease is characterized by chronic inflammation in the oral tissues, which releases pro-inflammatory mediators into the bloodstream. This systemic inflammation was implicated in the pathogenesis of various gastrointestinal disorders, including inflammatory bowel disease as well as irritable bowel syndrome. By reducing oral inflammation through periodontal therapy, it is possible to mitigate systemic inflammation and potentially alleviate symptoms of gut-related conditions.6
Periodontal disease induces gut microflora dysbiosis via salivary microbiota
In a latest clinical study, periodontitis can lead to an imbalance in gut microbiota as well as inflammation in the intestines through the movement of salivary bacteria. Fecal and salivary samples were obtained from 16 individuals without periodontal issues (PH group) as well as 21 individuals with severe periodontitis (SP group) and analysed using 16S rRNA (16S ribosomal RNA) sequencing. Major variations had been noted in both groups. Significantly, a higher presence of microbes originating from saliva was spotted in the SP group’s fecal samples. Following the transplantation of the residual salivary microbes into the C-PH as well as C-SP groups of C57BL6/J mice, it had been discovered that the composition of gut microbiota of the C-SP group differed substantially from that of the C-PH group, with Porphyromonadaceae as well as Fusobacterium was found to be notably more abundant in the C-SP group. The C-SP group exhibited substantially lowered crypt depth as well as expression of zonula occludens-1 in the colon. In the C-SP group, there was a considerable surge in the expression levels of mRNA of tight junction proteins, chemokines, and pro-inflammatory cytokines. Salivary microbiota had been tagged with CFDA-SE (Carboxyfluorescein Diacetate Succinimidyl Ester) and then transferred in mice to investigate if bacteria of saliva could endure in the intestine. It had been discovered that salivary microorganisms from the SP as well as PH groups.2
The current study's findings reinforced the significance of maintaining a healthy periodontal state. Moreover, optimizing our comprehension of the impact of periodontitis on the gut microbiota depends on understanding the process behind the transfer of salivary bacteria to the gut. Significantly, treating periodontitis may offer a fresh approach to managing systemic illnesses linked to the resistant gut microbiota.2
Conclusion
Periodontal healing may benefit gut health by modulating gut microbiota composition and reducing systemic inflammation. These results highlight the need for regular dental checkups and oral hygiene for both preserving oral health and enhancing general well-being. To fully understand the intricate interactions between the gut and oral microbiomes and to investigate potential treatment approaches that target both systems, more research is required.1
Editorial note:
References
- Anurag Satpathy: Periodontal healing by improving gut health. HTAJOCD 2023 March-April (4):10-13.
- Bao J,Li L,Zhang Y,Wang M,Chen F,Ge S, Chen B,Yan F. Periodontitis may induce gut microbiota dysbiosis via salivary microbiota. International Journal of Oral Science 2022; 14:32.
- Elzayat, H.; Mesto, G.; Al-Marzooq, F. Unraveling the Impact of Gut and Oral Microbiome on Gut Health in Inflammatory Bowel Diseases. Nutrients 2023, 15, 3377. https://doi.org/10.3390/nu15153377
- Talita Gomes Baeta Lourenςoa, Sarah J. Spencerb, Eric John Alm, Ana Paula Vieira Colombo. Defining the gut microbiota in individuals with periodontal diseases: an exploratory study. Journal of Oral Microbiology 2018; 10:1487741.
- Huang Y, Liao Y, Luo B, Li L, Zhang Y and Yan F (2020) Non-surgical Periodontal Treatment Restored the Gut Microbiota and Intestinal Barrier in Apolipoprotein E−/− Mice With Periodontitis. Front. Cell. Infect. Microbiol. 10:498. doi: 10.3389/fcimb.2020.00498
- Di Stefano, M.; Santonocito, S.; Polizzi, A.; Mauceri, R.; Troiano, G.; Lo Giudice, A.; Romano, A.; Mascitti, M.; Isola, G. A Reciprocal Link between Oral, Gut Microbiota during Periodontitis: The Potential Role of Probiotics in Reducing Dysbiosis-Induced Inflammation. Int. J. Mol. Sci. 2023, 24, 1084. https:// doi.org/10.3390/ijms24021084
Topics:
Tags:
Periodontitis is a chronic oral inflammatory condition, commenced by the accumulation of pathogenic dental plaque biofilm above and below the gingival ...
At least 50% of the onset of autoimmune diseases is attributed to unknown causes (1). Many retrospective studies have shown that most autoimmune disease ...
The human body consists of distinct and abundant microorganisms referred to as the microbiome [1]. The oral cavity is colonized by 700 different species of ...
In recent decades, we have recognized the vital role of microbiota in health and disease. The human gut and oral microbiota, the body’s largest ...
The last decade has witnessed a global rise in antibiotic resistance, creating substantial challenges for healthcare systems worldwide. While the primary ...
Live webinar
Mon. 23 February 2026
1:30 pm IST (New Delhi)
Ass. Prof. Elizabeth Shick, Dr. Zehra Yonel
Live webinar
Tue. 24 February 2026
11:30 pm IST (New Delhi)
Prof. Dr. Markus B. Hürzeler
Live webinar
Wed. 25 February 2026
1:30 am IST (New Delhi)
Prof. Dr. Marcel A. Wainwright DDS, PhD
Live webinar
Wed. 25 February 2026
9:30 pm IST (New Delhi)
Prof. Dr. Daniel Edelhoff
Live webinar
Wed. 25 February 2026
11:30 pm IST (New Delhi)
Live webinar
Thu. 26 February 2026
6:30 am IST (New Delhi)
Live webinar
Tue. 3 March 2026
9:30 pm IST (New Delhi)
Dr. Omar Lugo Cirujano Maxilofacial



 Austria / Österreich
Austria / Österreich
 Bosnia and Herzegovina / Босна и Херцеговина
Bosnia and Herzegovina / Босна и Херцеговина
 Bulgaria / България
Bulgaria / България
 Croatia / Hrvatska
Croatia / Hrvatska
 Czech Republic & Slovakia / Česká republika & Slovensko
Czech Republic & Slovakia / Česká republika & Slovensko
 France / France
France / France
 Germany / Deutschland
Germany / Deutschland
 Greece / ΕΛΛΑΔΑ
Greece / ΕΛΛΑΔΑ
 Hungary / Hungary
Hungary / Hungary
 Italy / Italia
Italy / Italia
 Netherlands / Nederland
Netherlands / Nederland
 Nordic / Nordic
Nordic / Nordic
 Poland / Polska
Poland / Polska
 Portugal / Portugal
Portugal / Portugal
 Romania & Moldova / România & Moldova
Romania & Moldova / România & Moldova
 Slovenia / Slovenija
Slovenia / Slovenija
 Serbia & Montenegro / Србија и Црна Гора
Serbia & Montenegro / Србија и Црна Гора
 Spain / España
Spain / España
 Switzerland / Schweiz
Switzerland / Schweiz
 Turkey / Türkiye
Turkey / Türkiye
 UK & Ireland / UK & Ireland
UK & Ireland / UK & Ireland
 International / International
International / International
 Brazil / Brasil
Brazil / Brasil
 Canada / Canada
Canada / Canada
 Latin America / Latinoamérica
Latin America / Latinoamérica
 USA / USA
USA / USA
 China / 中国
China / 中国
 Pakistan / Pākistān
Pakistan / Pākistān
 Vietnam / Việt Nam
Vietnam / Việt Nam
 ASEAN / ASEAN
ASEAN / ASEAN
 Israel / מְדִינַת יִשְׂרָאֵל
Israel / מְדִינַת יִשְׂרָאֵל
 Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
 Middle East / Middle East
Middle East / Middle East


















































To post a reply please login or register